Patient Radiation Safety in CT: What You Need To Know

In this week’s video, Eric from Olympic Health Physics explains the 10 pearls of radiation protection of patients in CT, as recommended by the IAEA (International Atomic Energy Agency) for the Radiation Protection of Patients (RPOP). This help will give some guidance on the best ways that we can employ to protect our patients when using computed tomography imaging.
1. Perform The Scan Only If It's Indicated
Try to avoid any unnecessary exams.
Remember that the lowest radiation exposure to a patient is the radiation exposure that doesn’t occur. This is why it’s important to know that if there’s an exam that shouldn’t be performed, then we shouldn’t be scanning the patient.
2. Consider The Use of Alternative Imaging Options
You can use alternative modalities to potentially answer the same clinical question.
Ultrasound or MRI don’t use radiation and they could be alternatives depending on the diagnostic question that’s trying to be answered. If a patient can be imaged using ultrasound or MSI from a radiation dose perspective, then it can be an excellent option when those modalities are appropriate.
3. Always Check If Your Patient May Be Pregnant
We don’t want to unknowingly image or do a CT on someone who is either pregnant or potentially pregnant. That’s the reason why you always need to verify the patient, whether or not they could be pregnant before doing their exam.
You can do this by having postings in the department that say, “Please notify the technologist if there’s a possibility that you’re pregnant”. Another option is to directly ask the patient if there’s any possibility that they could be pregnant.
4. Start Using Images With Some Noise Without The Loss of Diagnostic Information

It’s important to know that high-quality, detailed, and crisp images look really nice, but they may not be necessary for answering the diagnostic question.
You could potentially use a lower radiation dose and still answer the diagnostic question. The trade-off is that we’re going to introduce some noise and potentially lose some image quality. However, that loss and image quality are not going to necessarily change the diagnosis or the outcome for the patient.
We want to make sure that you’re using the right radiation dose for answering the clinical question.
5. Use Indication-Specific CT Protocols For Each Body Part
We want to use indication-specific protocols where they’re applicable. For example, not every chest CT should be a full chest image. We could do a low-dose screening, a lung screening chest protocol, and also potentially do a low-dose nodule follow-up protocol.
We want to use very specific protocols for the type of exam that we’re trying to do. The reason is that oftentimes those very specific protocols can be acquired at a lower radiation dose to the patient.
6. Multiple Pass or Multiphase CT Should Not Be Performed Routinely
It’s important to know that multiple pass or multiphase CT should not be performed routinely. We want to try to limit the amount of passes that we make through the patient. Only do the passes that are actually necessary and potentially combine different protocols.
This is why multiphase CT studies can often be 2 to 3 times the amount of radiation dose as just a regular CT.
7. Adjust Exposure Parameters According To The Patient And Body Part
We want to adjust the technique that we’re using to image our patient for the actual patient size. First, we want to take into account the size of the patient and the exam. Then, adjust any technique that we’re using so it’s specific to the patient and the body part that we’re imaging.
The reason for this is to get away from a one size fits all technique and move to very patient-specific techniques. That way, smaller patients receive lower radiation doses than larger patients.
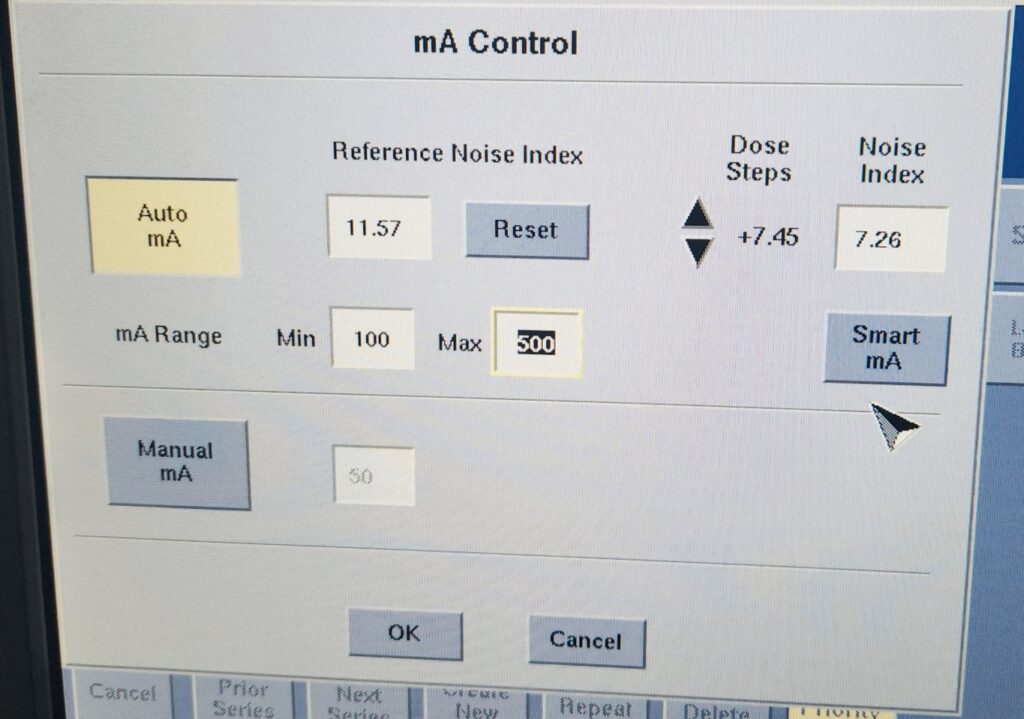
8. Know Your Equipment, Including the AEC System
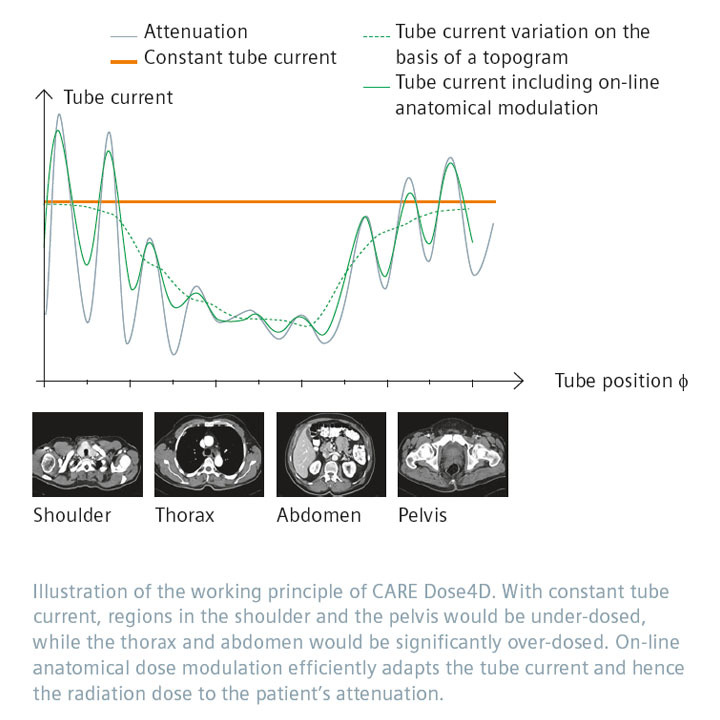
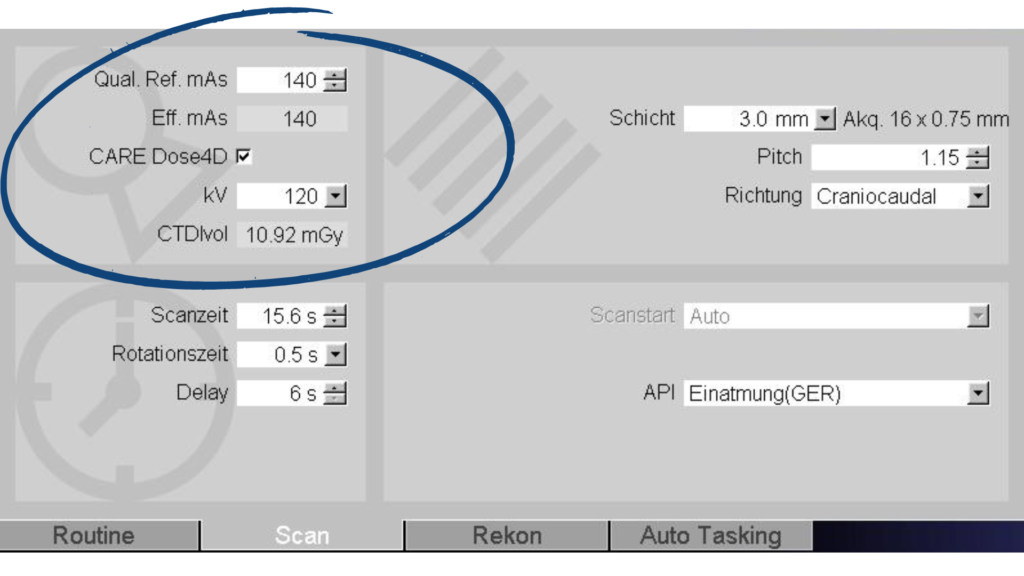
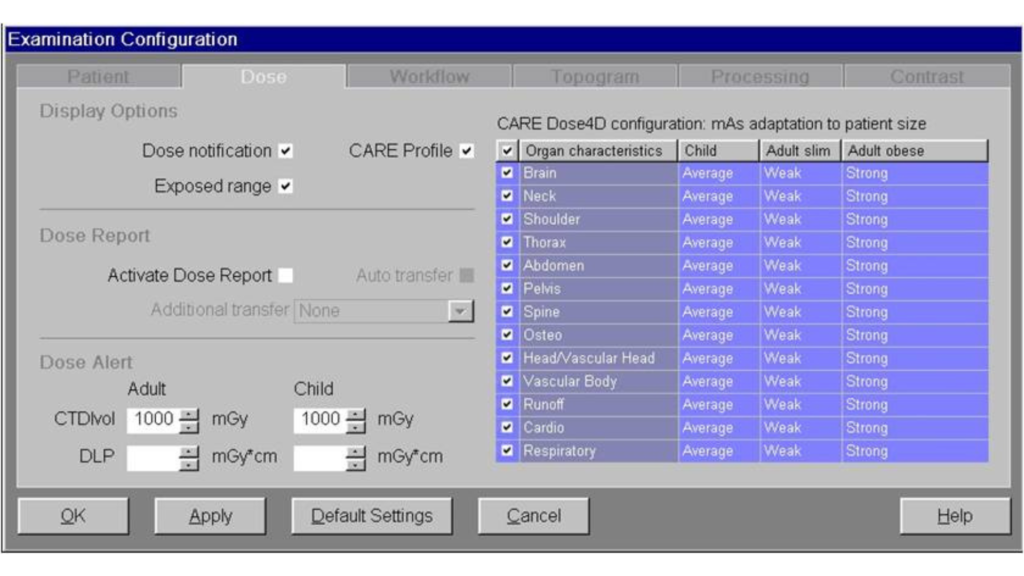
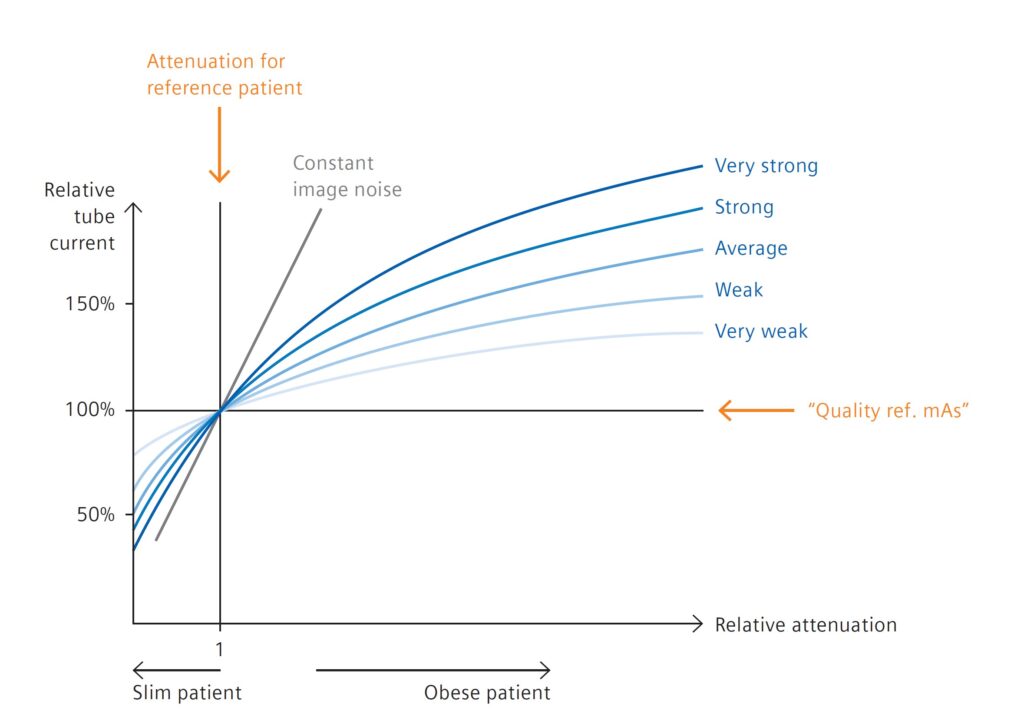
Another important aspect is to know your equipment. For example, understand how the AEC (Automatic Exposure Control) works or the tube current modulations and how that works for your system.
How Does CARE Dose 4D Work?
If you’re scanning on a Siemens scanner, make sure you understand CARE Dose4D. And if you’re scanning on a GE scanner, make sure you know how AutomA works. This way you can use the scanner to the best of its ability and it will help you give the right radiation dose to your patient.
To learn more about the Siemens CARE Dose4D system, check out our previous post here. And for information on the GE AutomA system, you can find our latest post here.
9. Use Good Technique
Use good technique when we’re talking about good technique. These are things like:
• Making sure that your patient is iso-centered within the gantry. This is in both the lateral direction as well as the AP direction.
• Confirm that the patient is iso-centered, particularly while using tube current modulation.
• Check that your scan length is covering only the anatomy that’s absolutely necessary. We don’t want to scan the diagnostic portion of the CT.
The one caveat to this is with a scout. When using a scout, it’s better to use a little bit longer of a scout than what you intend to cover with your diagnostic scan. Keep in mind that he diagnostic scan should be shorter than your scout.
10. Pay Attention To Radiation Dose Values
Don’t forget to pay attention to your radiation dose values, such as the pre-scan CT because you need to make sure that you’re falling within your pre-determined dose values and dose limits.
Review the doses that you’re using on a monthly basis to see if there are any adjustments that you can make. Consider things like your protocols, your techniques, and how you’re scanning patients. From this information, you can have a pretty good idea of what your doses should actually be, what they have been and what they should be for the equipment that you’re using as well as for what your radiologists are accustomed to looking at.
Now you know that there are ten different ways to protect your patients, reduce their radiation dose and make sure that they’re getting the right radiation dose for the type of exam that’s been ordered.
Click here to download your copy of the IAEA’s 10 Pearls of Radiation Protection of Patients in CT.
Our team is dedicated to ensuring that your facilities’ radiation safety program functions in accordance to regulatory standards, sound radiation safety principles, and most importantly serves to protect staff, patients, and the general public from the hazards associated with ionizing radiation. To this end, Olympic Health Physics can provide a physicist to your organization to fulfill the Duties of the Radiation Safety Officer. To learn more, check out our RSO Services or click the link below.