A Guide to Surviving an NRC Inspection
A Nuclear Medicine Technologist’s Guide to Surviving an NRC Inspection
As a CNMT, or Nuclear Medicine Technologist, you have many responsibilities in your job. You’re preparing and administering radioactive substances, helping patients during test procedures, and ensuring a safe working environment for yourself and those around you.
The one aspect of the job that many Nuclear Medicine Technologists dread is a facility or site inspection from the NRC, or Nuclear Regulatory Commission.
Watch the video above on our YouTube channel as Eric walks you through five tips for preparing and surviving an NRC inspection
What Is The NRC?
The NRC or Nuclear Regulatory Commission is the governmental regulatory body ensuring public safety and industry standards for all uses of nuclear and radioactive materials and processes within the United States. This includes academic, medical, and industrial usage of radioactive products.
How Often Can You Expect An Inspection From The Nuclear Regulatory Commission?
The Nuclear Regulatory Commission has several regional offices. The NRC usually conducts unannounced inspections periodically for licensed activities. The inspector identifies whether the licensees are performing activities in accordance with the regulatory and license requirements. The results of the inspection are provided to the facility in written form. The report may contain enforceable actions or follow up items for re-inspection. All NRC inspection reports are also made available to the public through its electronic document retrieval system.
How To Survive An NRC Inspection
There are several key things to remember when remaining prepared for an NRC inspection. Here are our top five tips:
Tip #1: Keep Good Records
Remember that your inspection starts before the inspector ever arrives. Maintaining good records and keeping them all in one location will make it easier for the inspector to review your radiation safety program and associated documentation.
Examples of required regulatory documents can include:
• Surveys
• Leak tests
• Sealed source inventory lists
• Dosimetry records
• Internal written directives
• Radioactive waste records
• Radiation safety committee meeting minutes
• Well counter quality control reports
• Survey meter calibration certificates
Having all records clearly organized can help the inspection process go more smoothly for the NRC inspector. If you make the process go efficiently for the inspector, they’re more likely to go through your records a bit more quickly and move on to other parts of the inspection.
Tip #2: Be Truthful
It’s essential that you’re truthful with the inspector. There are really bad things that can happen if you’re not truthful with the inspector, particularly if you knowingly and willingly providing false documentation or false records.
However, you also don’t want to overshare. So only give the inspector the records that they’re asking for and let them see the processes that they want to see. This will help your inspection process go more effortlessly.
Tip #3: Practice Good Radiation Safety Techniques
While it’s important at all times to practice good radiation safety techniques, it’s particularly critical in front of an NRC inspector.
Here is a reminder of several important radiation safety techniques:
• Use syringe shields
• Draw up doses behind an L block
• Assay doses in the dose calibrator
• Wear your lab coat
• Wear protective gloves
• Be sure to wear your own dosimeter
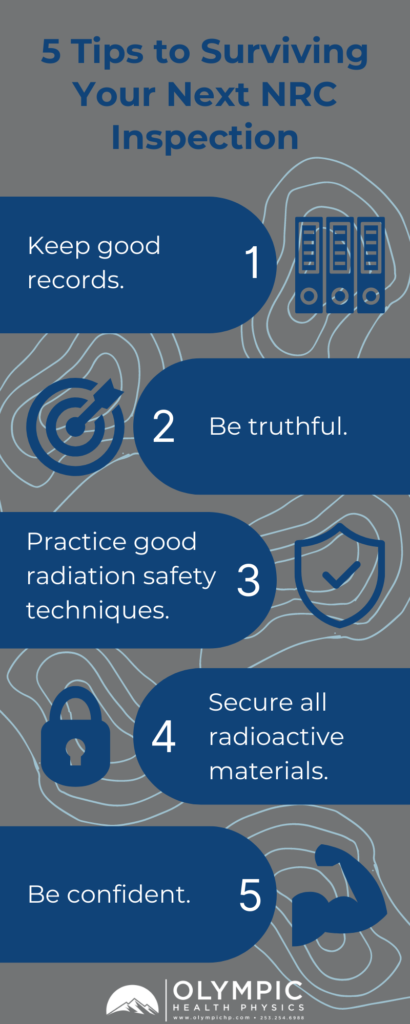
Tip #4: Secure All Radioactive Materials
Make sure to secure all radioactive materials. What does that mean?
Here are a few examples:
• Keep your hot lab door closed
• When drawing up doses in preparation of a later injection, keep them safe in a secured room or under constant surveillance

Tip #5: Be Confident
No one knows your department like you know your department. You know everything that is going on within your department. You know where your records are at. You know where you have processes that you could improve upon. So be confident in what you are presenting to the inspector. And if you’re running a good radiation safety program, the inspection should go very smoothly.
Implementing these five tips in your nuclear medicine department can help ensure an efficient and painless NRC inspection. If you have questions or comments about any of the ways that you can best prepare for an NRC inspection or a state inspection if you’re in Agreement State, feel free to drop us a comment or send us an email. We’ll be happy to take a look at your program and figure out ways that you can be best prepared for your next regulatory inspection.
Your medical physicist is a great resource for you when designing your Radiation Safety Program. You can also always reach out to us if you have questions or want more information on Radiation Safety or want to see why you should partner with us. We also offer Radiation Safety Officer Services, Radiation Dose Optimization, and Health Physics Services.